How Florida Asset Protection Works
What Is Florida Asset Protection?
Asset protection is the legal strategy of structuring assets to shield them from lawsuits, creditors, and judgments. It uses tools like trusts, LLCs, and exemptions. Effective asset protection plans reduce financial risk by making it harder for a judgment creditor to collect.
It can improve a debtor’s ability to settle issues as well.
It is rarely too late to protect assets from creditors. Some strategies are viable even after a lawsuit is filed and or a judgment is entered. Still, asset protection is more effective if done before liability arises.
Florida is considered one of the best states for asset protection because of its generous creditor exemption laws. Florida law protects an unlimited amount of homestead equity, tenants by entireties property, head of household wages, retirement accounts, annuities, life insurance, and disability insurance.
How Does Florida Asset Protection Work?
In our experience, everyone fortunate enough to accumulate assets in today’s economy needs asset protection.
In the United States, there are more than one million lawyers, each with a license to file lawsuits against deep-pocket defendants. Too often, decisions by judges or juries are based more on emotion than on facts, and frivolous lawsuits result in a catastrophic damage award that wipes out a lifetime of hard work and investment.
If a judgment is entered against you in Florida, the judgment creditor can find out your financial information and begin to collect on the judgment. Asset protection uses legal methods to better protect what you have and your income from collection of the judgment.
Florida law is debtor-friendly because of the numerous assets exempt from lawsuits and civil judgments. The strength of Florida’s debtor-friendly laws stems from three legal sources:
- The Florida Constitution
- Florida statutes
- Florida common law

Florida Constitution
The Florida Constitution is the most fundamental Florida legal document, and it sets forth Florida’s most important protections, including Florida’s well-known homestead protection.
Florida Statutes
The Florida legislature has enacted many laws that protect various types of assets from creditors of Florida residents. There are also statutes providing creditors with tools to collect judgments.
Florida Common Law
There are protections based on what is referred to as common law or legal tradition. Common law is established by appellate judges in individual cases, and their decisions become precedent for future cases with similar issues.
Courts create common law Florida asset protection through their interpretation of Florida’s Constitution and statutes. Consistent interpretations become part of common law legal tradition and are deemed “settled law.” Judges are supposed to apply common law precedent because the underlying common law principles are in the Florida Constitution or Florida statutes.
Update for 2025
The year 2025 is not bringing any major changes to Florida asset protection law and strategies. In our view, appellate decisions in 2024 mostly upheld longstanding exemptions used by Florida debtors.
We help protect what you’ve earned.
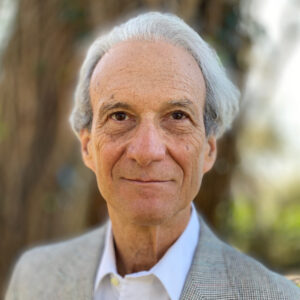
Jon Alper and Gideon Alper are nationally recognized experts in asset protection planning and implementation. In over 30 years, we have advised thousands of clients about how to protect their assets from judgment creditors.
We provide all services remotely by phone or Zoom.

Types of Exempt Assets in Florida
- Homestead property, with some acreage limitations.
- The wages of someone who qualifies as head of household.
- Annuities.
- Life Insurance cash value.
- Retirement Accounts. For example: an IRA or 401k.
- Tenants by entireties property when the judgment is against one spouse in a marriage.
- Interest in a multi-member LLC with a properly written LLC operating agreement (but still subject to a charging lien).
- Disability income.
- $1,000 of value in a vehicle.
- $1,000 of personal property (or $4,000 if you do not own a home).
- Prepaid college plans.
- Various generic exemptions, such as health aids, medical savings accounts, and unemployment benefits.
- Social security under federal laws.
- Some properly drafted estate planning trusts protect the beneficiaries’ interest and inheritance from their creditors.
Homestead Protection
The most well-known exemption in Florida is the the Florida homestead exemption. The protection is provided by Article X, Section 4 of the Florida Constitution.
A key feature of the Florida homestead exemption is the ability of a judgment debtor to at any time make transfers or conversions into a protected homestead without regard to fraudulent transfer liability. In other words, a judgment debtor in Florida can, even after a judgment, purchase and move into a large homestead in a clear effort to avoid collection from creditors, and the creditor has no recourse.
The Florida Constitution exempts an unlimited value of homestead property. There are limitations on the size of the homestead property:
- 1/2 acre lots within a municipality
- 160 acres in the unincorporated county (applies even if the property started off in the city limits but was later annexed)
- The protection applies to separate but contiguous lots within the size limit.
In addition to the constitutional protection of homestead property, married couples typically acquire homestead together, giving them the protection of tenancy by the entireties ownership.
For families that own a house greater than 1/2 acre inside the city limits, some advanced asset protection techniques can allow a judgment debtor to protect the entire equity using a series of transfers and leases.
Homestead protection requires actual residence in the home. Most importantly, it is not enough that a judgment debtor intends to live in the property at some point in the future (for example, if the property is under construction). Proceeds from the sale of a homestead are exempt from creditors so long as the judgment debtor intends to reinvest the proceeds into a new Florida homestead within a reasonable amount of time.
Tenants by Entireties
A basic asset protection exemption for married Florida debtors is to own property as tenants by the entireties. Tenants by entireties refers to joint property owned by a married couple as an indivisible fictional unit. Title cannot be severed without the consent of both spouses in most circumstances. Assets held as tenants by entireties are generally immune from collection from a civil creditor of just one spouse.
Tenants by the entireties is a common law protection rather than a Constitutional or statute-based exemption. Tenancy by the entireties was developed from British common law and thereafter adopted by many U.S. states in the mid-1800s. However, only a few states today recognize tenancy by the entireties. Some of these states limit entireties ownership to real property. In Florida, all personal and real property can be held as tenants by the entireties.
Mere joint ownership of an asset by husband and wife is not enough for property to qualify as tenants by entireties. The ownership must meet the “six unities,” which include unity of possession, unity of interest, unity of time, unity of title, survivorship, and unity of marriage. So long as there is not an existing creditor issue, couples should consider transferring any assets held jointly or individually before their marriage to themselves as tenants by entireties after marriage.
Tenants by Entireties Bank Accounts
Opening a tenants by entireties bank account requires attention to legal detail. A joint bank account that is not opened jointly by both spouses at the same time, and in the same document, is not an entireties account. Furthermore, if the bank offers a box on the signature card for tenancy by the entireties ownership, then the married couple must have checked that box in order to have entireties ownership.
Once an account fails in any way to meet entireties requirements, it cannot be fixed. The couple must open a new account—while keeping in mind fraudulent conveyance considerations.
Tenants by Entireties Presumptions
With real estate, and to a lesser extent with bank accounts, tenancy by the entireties ownership is presumed even if there is no language specifying tenancy by the entireties ownership. But this presumption is not applicable to LLCs, partnerships, or corporations. These business entities strongly benefit from specific language in their governing agreements and certificates to indicate entireties ownership.
Note that assets held as tenancy by the entireties can be freely transferred to a non-debtor spouse without incurring fraudulent transfer liability because there can be no fraudulent transfer of an exempt asset. One relevant case is In re Blatstein, 192 F.3d 88 (3rd DCA 1999).
Life Insurance and Annuity Contracts
The cash value of life insurance proceeds is protected from the policy owner’s creditors. The policy must insure the owner’s own life for the protection to apply.
Unlike inherited pension plans and IRAs, life insurance proceeds are not protected in the hands of a beneficiary from that beneficiary’s creditors. The exemption statute protects the life insurance owner, not the ultimate beneficiary, from judgment creditors.
In the case of annuities, the exemption statute expressly protects annuity proceeds including proceeds deposited in a bank account. A judgment debtor should segregate the annuity payments or otherwise be able to clearly trace bank funds to the annuity.
Head of Household Wages
Other than tenants by entireties and homestead, the major protection from creditors in Florida is the unlimited head of household wage exemption.
The wages of a debtor who is head of household are exempt from creditor collection. This exemption extends to wages deposited in a bank account for up to six months. If the account contains non-wage money as well, the debtor will have to show which funds are actually wages in order to claim the exemption.
A head of household is someone who provides more than 50% of the support for someone else. The debtor must have a moral or legal obligation to support the other person. Common examples are a spouse, child, parent, or another relative.
Protection of the wages becomes more difficult when the debtor is earning wages from their own company. It’s critical in these situations to document the employment relationship with an arms-length employment agreement and to pay actual wages periodically. Courts have denied head of household protection when the debtor controls the timing and amount of salary from the employer.
Retirement Accounts
Pension plans (401k) and IRAs are exempt from creditors under federal and Florida law. The protection has an added benefit in that the funds in the accounts enjoy tax-deferred growth.
Business owners should consult with a financial advisor or an accountant to determine what type of retirement plan is available. The answer may be different depending on the number of employees in the business.
Some states do not exempt IRAs from creditors. Individuals in these states can still exempt IRAs in bankruptcy. Often this means that non-Floridians resort to bankruptcy in order to protect sizeable IRA accounts because the accounts would otherwise not be protected.
Inherited IRAs are similarly protected from creditors in Florida. However, sometimes people in Florida have children in other states that do not protect inherited IRAs. In these situations, children that have their own creditors would most likely not be able to use Florida law to protect the inherited IRAs. If the parents leave the out-of-state beneficiary’s share to a trust, the trust’s spendthrift provisions would protect the child’s inherited IRA from the child’s creditors.
Prepaid Tuition and 529 Accounts
A 529 account is a tax-advantaged account designated for educational expenses. Funds in the account grow tax-free and are not taxed when withdrawn if they are used for an approved expense category. Some states, such as Florida, offer a pre-paid college tuition program. These programs allow residents of the state to pay a set amount to cover college expenses in the future, no matter how high tuition increases.
Florida law fully protects 529 accounts and pre-paid college programs from judgment creditors. The protection is valid even if the plan owner is permitted to spend the funds on themselves (with tax penalty). The protection extends to money withdrawn from the plan. For example, a person may withdraw money from a 529 plan with the intent to pay an education expense and deposit the funds in a segregated bank account where the funds remain protected.
Personal Property
Personal property includes your car, furniture, computers, phones, and even your family pets. In short, there is no significant exemption for personal property. Very aggressive creditors could seek a sheriff’s levy to seize your personal assets for public sale. Some creditors threaten levy on personal property to gain leverage, but in practice, the levy does not occur in most collections. Creditors infrequently go after personal property because the costs of sheriff levy, storage, insurance, and auction are not warranted when the property has little value at auction.
Some personal property is exempt. Medical devices being used to treat a diagnosed condition are exempt from creditors. The exemption can even apply to vehicles, such as vans, modified for an actual health condition. In some cases, a debtor owns particularly valuable personal property such as artwork, jewelry, and antiques. These debtors better protect their valuable personal property using tenants by entireties ownership, LLCs, or advanced estate planning techniques.
Quasi-Exempt Assets in Florida
Quasi-exempt assets are those assets that are not exempted by statute, but are still mostly protected from creditors for other reasons. The most common of these are limited partnerships and limited liability companies that are used for asset protection of businesses or investment assets.
LLC and Limited Partnerships
Under Florida law, a creditor’s sole remedy to collect a debtor’s interest in a multi-member LLC or limited partnership is a charging order. A charging order is a court-ordered lien on the distributions from the LLC to the member.
Because the charging order is an exclusive remedy, the creditor cannot get the underlying assets owned by the company, thereby protecting these assets from execution.
With a properly drafted operating agreement, an LLC can prevent a creditor with a charging lien from receiving any distributions even if the LLC or partnership generates profits.
Note that an LLC must be a multi-member LLC for the charging order protection to apply. Single-member LLCs are not protected. The creditor can force the sale of the entire LLC interest. The inability of a creditor to get anything more than a charging order against a multi-member LLC or partnership gives a judgment debtor a strong negotiating position in settlement discussions. A charging order is difficult to enforce, and a patient judgment debtor can delay or stop distributions indefinitely.
Asset Protection Trusts
Some states have made laws allowing the formation of domestic asset protection trusts (DAPT). These are self-settled trusts that are protected from judgment creditors by state statutes. In Florida, self-settled trusts are not protected from creditors. Several Florida court decisions have expressed the state’s public policy against self-settled asset protection trusts.
The best-known domestic asset protection trust states are Wyoming, Nevada, Delaware, and Alaska. Over the years, many websites have promoted the benefits of asset protection trusts in these states.
Florida debtors should be cautious before setting up an asset protection trust in these DAPT states. It is uncertain which state’s law would apply in a Florida court should a creditor seek to collect the assets in a DAPT formed outside of Florida. Some courts have held that no matter where a DAPT is formed, Florida law—not the law of the trust formation state—applies.
Offshore LLCs and Trusts
An offshore trust is a self-settled trust formed under the laws of a foreign jurisdiction, usually the Cook Islands. A common plan involves an offshore trust in one jurisdiction that owns an offshore LLC in another jurisdiction. The offshore LLC then owns the underlying assets.
Cook Islands trust law has some of the best anti-creditor provisions in the world, and the jurisdiction is frequently regarded as the gold standard of offshore asset protection. Under Cook Islands law, the assets of the trust are unavailable to creditors of the trust beneficiary so long as the trust was funded two years before the claim arose.
Like many asset protection techniques, offshore trusts are most effective when the trust is funded before a claim arose. Some bankruptcy and federal court judges have been able to force an aggressive judgment debtor to bring back assets located in an offshore trust when the court believes the debtor is trying to hide assets from creditors.
That said, creditors with relatively small state court judgments may not want to invest the significant legal fees required to attack an offshore trust plan, even if the debtor transferred assets to the trust after liability arose.
Protected Bank Accounts
Certain domestic bank accounts in the U.S. are unable to be garnished under state law. The law does not explicitly exempt the debtor’s funds in the bank account from collection, but the creditor’s inability to garnish the bank makes judgment collection extremely difficult.
Fraudulent Conveyance
The central issue in asset protection planning is almost always the threat of a fraudulent transfer or fraudulent conversion claim
A fraudulent transfer is a conveyance of title or ownership by the judgment debtor for the purpose of avoiding collection by the judgment creditor. A fraudulent conversion is the debtor’s conversion of a non-exempt asset to an exempt or protected asset. An example is moving money in the debtor’s individual account to a tenants by entireties joint account. Fraudulent conveyance often refers to both transfers and conversions.
Fraudulent transfer allegations are more common issues than fraudulent conversion claims. One reason is that conversions to an exempt homestead are protected from claims of fraudulent conversion.
If a creditor successfully argues that the debtor has made a fraudulent conveyance, the creditor can have the court void or undo the conveyance, or the creditor may seek a judgment against the recipient of the fraudulent transfer for the value of the asset received.
A fraudulent conveyance allegation is nothing more than a judgment collection remedy. The pertinent statutes does not give a creditor the right to additional damages or attorney fees.
The word “fraudulent” in fraudulent conveyance does not mean that the action is illegal. A fraudulent conveyance in a civil collection context is not the same thing as civil or criminal fraud.
Elements of a Fraudulent Transfer
Under section 726.105 of Florida law, a transfer is fraudulent if:
- it was made with actual intent to hinder, delay, or defraud any creditor of the debtor; or
- it was made was made without receiving a reasonably equivalent value, and the debtor was engaged or about to engage in a business or transaction for which the remaining assets of the debtor were unreasonably small in relation to the business, OR the debtor intended to incur, or believed or reasonably should have believed that he or she would incur, debts beyond the ability to pay as they became due.
The first element is hard to prove as it involves the debtor’s state of mind. Therefore, courts rely on a list of intent factors (or “badges of fraud”) that indicate what the debtor intended. The more that these factors exist for a given transfer, the more likely it is that a judge will find that the transfer was fraudulent under the statute.
Badges of fraud for a fraudulent transfer include:
- The transfer or obligation was to an insider.
- The debtor retained possession or control of the property after the transfer.
- The transfer or obligation was disclosed or concealed.
- Before the transfer was made or obligation was incurred, the debtor had been sued or threatened with suit.
- The transfer was of substantially all the debtor’s assets.
- The debtor absconded.
- The debtor removed or concealed assets.
- The value of the consideration received by the debtor was reasonably equivalent to the value of the asset transferred or the amount of the obligation incurred.
- The debtor was insolvent or became insolvent shortly after the transfer was made or the obligation was incurred.
- The transfer occurred shortly before or shortly after a substantial debt was incurred.
- The debtor transferred the essential assets of the business to a lienor who transferred the assets to an insider of the debtor.
If the judgment creditor wants to pursue a fraudulent transfer claim, it must usually do so within four years, or one year after the transfer could have been reasonably discovered.
Common Sources of Liability in Florida
Before considering any asset protection strategies, a person should first recognize the most likely sources of liability. A person can face legal liability for a variety of liability events, including:
- Professional malpractice
- Automobile accidents
- General debt, including credit cards and medical bills.
- Premises liability. This refers to liability stemming from ownership of a building. For example, someone slips and falls on the premises. Or, a tenant is injured from an error made by a property manager.
- Liability stemming from relationships. This type of liability includes co-signing on loan applications, for example. Some people face civil claims from former partners in personal relationships.
- Employment liability. An employer is generally liable for the acts of employees when they act in the scope of their employment.
- Intentional torts. People are often sued for alleged physical assault, racial or sexual discrimination, or defamation in social media.
Among the most common of the above concerns are liability stemming from professional malpractice and from automobile accidents.
Professional Malpractice
A professional malpractice suit occurs when a client, or former client, files a lawsuit against the professional, claiming that the professional’s negligence damaged the client physically, financially, or emotionally. Doctors, lawyers, and accountants are all exposed to malpractice claims in their line of work.
The threat of a malpractice suit puts the professional at a higher risk of legal liability compared to most individuals. This is more true if the professional also owns a business for the professional practice.
As a result, it is even more important for professionals to engage in early asset protection planning.
Automobile Accidents
Liability for car accidents is not just limited to the driver causing an accident. The car owner is responsible for the negligence of any permitted driver. For example, if a person owns a vehicle driven by their spouse, and the spouse causes an accident, both spouses are liable for injuries caused by the driver’s negligence.
In addition, under Florida law, a minor with a learner’s permit or license must have an adult agree to be held liable for the minor’s negligence. If a parent signs the minor’s application for a learner’s permit or license, then the parent is liable for the minor’s negligent driving.
In a situation where one spouse has more at-risk assets or income, the spouse with less at risk should sign the child’s license application. Fortunately, the designation of the responsible parent can be changed. Furthermore, a business owner or the business entity can be held liable for the negligence of employees driving their vehicles.
Credit Card Debt
Credit card debt is a primary factor leading to personal bankruptcy in Florida. Consumers facing job loss or medical bills often find themselves indebted to several credit card companies. These credit card creditors typically act aggressively to collect unpaid credit card bills. They may contract with professional debt collectors or file lawsuits against their credit card customers. Faced with an onslaught of litigation and nasty bill collectors, many credit card debtors believe that Chapter 7 bankruptcy is the only way to protect themselves.
Successful bankruptcy does wipe out all of a person’s credit card debt as well as any other unsecured debts including car loans, medical debt, and mortgage deficiency judgments. There are problems and risks involved in bankruptcy for many credit card debtors. Debtors have to pass a “means test” in order to qualify for bankruptcy. Bankruptcy causes debtors to forfeit all assets not exempt under bankruptcy law, and fewer assets are exempt in bankruptcy than in state court collection. Experienced and very competent bankruptcy trustees, working on a contingency fee, can challenge asset exemptions and pursue legal challenges to prior fraudulent transfers and preferential payments to creditors.
In Florida, most people facing credit card debt can avoid the risks of bankruptcy. Because Florida non-bankruptcy law protects assets and transfers that are vulnerable to a bankruptcy trustee these debtors can retain more assets and achieve favorable legal action by defending the credit card company collection through state court proceedings.
For example, Florida homestead law protects the owner’s homestead from creditors regardless of when the debtor acquired the homestead. The Florida Constitution places no monetary ceiling on homestead-protected property. Money used to purchase or improve a homestead cannot be challenged in state court as a fraudulent conversion even if the homestead was acquired or improved after the debtor was sued. Bankruptcy law protects only limited amounts of homestead equity acquired within 40 months of filing bankruptcy. The bankruptcy trustee may challenge and reverse the debtor’s purchase of a Florida homestead within 10 years of the bankruptcy filing.
Bankruptcy is not a good option for recent Florida residents. Florida’s generous homestead protection and other exemption laws apply to all Florida residents immediately upon the establishment of Florida residency. There is no waiting period for the benefits of Florida’s asset protection law. In bankruptcy, a new Florida resident cannot use Florida’s homestead exemption and other Florida protections for 24 months after moving to Florida. The new Florida resident has to use exemption law in the state of their former residence, and these laws are usually less advantageous in bankruptcy court.
Bankruptcy trustees are generally speaking more effective debt collectors than the collection attorneys who represent credit card companies. Bankruptcy trustees have jurisdiction over all of the debtor’s assets wherever located in the U.S. A credit card judgment is only good in the state where the lawsuit was filed, and the judgment does not affect the cardholder’s real estate or financial accounts situated in other jurisdictions.
Florida’s asset protection laws give credit card debtors the ability to protect most of their assets from credit card judgments outside of bankruptcy. Effective asset protection planning will enhance the debtors negotiating position with credit card companies. People who engage in asset protection instead of bankruptcy achieve better settlements and results than those who subject all their assets to examination and attack by a bankruptcy trustee.
Steps to Asset Protection in Florida
Asset protection planning in Florida is best done early. After a liability event occurs, your asset protection options decrease, and any asset protection plan is less effective because of fraudulent conveyance issues.
1. Consulting with an Asset Protection Attorney
Florida asset protection planning involves developing a customized plan with an attorney specialized in Florida exemption law to protect assets from lawsuits and collection of civil judgment. Asset protection has three steps:
- Reviewing the legal situation and circumstances of civil liability.
- Developing a comprehensive list of assets and income to determine what is currently protected or not protected.
- Evaluating legal options to better protect those assets from creditors.
2. Pre-Issue Planning
Engaging in asset protection planning before you expect legal liability is the best way to ensure your asset exemptions will hold up in court. Asset protection is perfectly legal, and individuals have the right to arrange their assets as they see fit, including protection against future claims.
The Florida Constitution states that Florida residents have a “basic right” to protect their property:
All natural persons, female and male alike, are equal before the law and have inalienable rights, among which are the right to enjoy and defend life and liberty, to pursue happiness, to be rewarded for industry, and to acquire, possess and protect property.
Protection of property reasonably includes protection from civil as well as physical threats.
Keep in mind that early asset protection planning does not simply mean planning before a lawsuit is filed. As soon as you believe you may be sued for a particular event that has already occurred you are in the realm of post-issue planning.
3. Post-Issue Planning
Most people don’t think about asset protection until after an unexpected adverse event. For instance, people cause a car accident, they encounter financial misfortune leaving them unable to pay a particular debt, they have a patient or client that had a bad outcome, and so on. There are effective asset protection tools available even after the liability issue first occurs.
The main problem with post-issue asset protection is the potential that asset titling or transfers can be undone as fraudulent conveyances. Carefully planned transfers done in the face of a legal threat may withstand fraudulent conveyance attack. For example, in most cases, Florida law permits the conversion of non-exempt assets to a homestead property even after a court enters a judgment. Transfers of non-exempt assets made for adequate consideration are also effective.
Asset Protection Difficulties
Divorce
Asset protection typically refers to protection from civil creditors. Asset protection tools are mostly ineffective to avoid paying family court judgments for alimony or child support.
Family law judges have more powers than judges in civil cases to enforce their family court judgments and orders. Family law judges can override state law protections for retirement accounts, asset protection trusts, state bank account protections, and even homestead in order to enforce family court decisions.
A court can hold a debtor in contempt for failure to turn over assets in a marital settlement or for failure to pay child support. To avoid contempt the debtor must often use assets that are otherwise exempt from civil judgment collection to pay alimony and support. This threat of contempt (and jail time) makes typical asset protection tools in a divorce context ineffective.
Not even offshore asset protection can save the day. Family law judges can order defendants to bring back trust assets to the United States. While an offshore trustee might not comply with the debtor’s request to send assets back, the judge can take various actions against the trust debtor until the debtor convinces the trustee to comply.
Features of property ownership, rather than state law exemptions, can still help protect assets from child support and spousal support claims. For example, if a divorced spouse remarries, newly acquired assets held as tenants by entireties with the new spouse may be immune from collection from the ex-spouse, even for support purposes.
Federal Agencies
Florida statutory exemptions are not effective against certain “super creditors” under federal law. These super-critors include the IRS, Department of Justice, SEC, FDIC, and FTC. Super creditors can seize assets that may be exempt under state law because federal debt collection rules and procedures supersede corresponding state law.
For example, the IRS and SEC can take half of the personal property that otherwise might be exempt as tenants by entireties. Federal agencies can garnish the salary of a Florida head of household. Federal agencies can also seize assets preemptively before a judgment is even entered against the Florida debtor. In this way, the federal agency substantially affects the ability of the debtor to retain legal help, which often forces a settlement favorable for the U.S. government.
Taxes
Asset protection planning usually does not shield tax debtors from U.S. income tax liability. The IRS has a tax lien on all the taxpayer’s assets to secure collection of delinquent taxes notwithstanding any state exemption (including Florida homestead). Still, some people mistakenly believe they can move assets offshore to protect the assets from IRS collection or from the income being subject to U.S. income tax. Do not confuse offshore asset protection planning with offshore tax planning. Offshore asset protection with after-tax money is legal. Moving assets offshore to avoid the recognition of income amounts to tax evasion. Offshore tax evasion is criminal.
Reducing Risk of Liability
The best and least expensive asset protection is common sense planning. For instance, liability insurance should often be the first line of defense against claims for negligence. Insurance provides you with the money to pay negligence claims without jeopardizing personal assets. Liability insurance includes auto insurance, malpractice insurance, homeowner’s insurance, and personal umbrella insurance.
Next, people can reduce legal risks and lawsuits by planning and minimizing unnecessary risks in their business and personal dealings. For example, people should not rely on oral promises and agreements in their business dealings as they often result in confusion and misrepresentation. Avoid getting involved in business and financial relationships with people you do not trust or with people who seem combative and adversarial.
Business agreements should be reviewed by a lawyer in advance. A few dollars spent on attorney fees before signing the contract can save substantial attorney fees in the future.
Cars
For most married couples, the primary driver should own each vehicle. This limits the potential of joint spousal liability stemming from one spouse causing an accident while driving the other spouse’s car. Cars should not be owned jointly by two spouses because both spouses are liable for negligence regardless of who was driving.
Remember that a judgment against both spouses will jeopardize otherwise protected assets owned jointly as tenants by entireties. LLC ownership of vehicles is also possible, but this could lead to higher insurance costs.
Boats
Under Florida law, the owner of a boat can be held liable for the negligence of the boat driver if the owner is physically on the boat at the time of the accident. Joint liability of spouses should be avoided for the same reasons discussed above pertaining to automobiles.
Larger recreational vehicles, including boats, airplanes, or other motorized transportation are sometimes better owned by a separate LLC. LLC ownership may increase insurance premiums.
Umbrella Insurance
Under Florida law, automobile owners must maintain an insurance policy with a minimum coverage of $10,000 per person for bodily injury. The minimum coverage is usually insufficient. Florida is a litigious state. There are many personal injury attorneys advertising to attract clients to sue for accident injury. Florida residents who have accumulated wealth should maintain the highest amount of personal liability coverage offered by their insurance carrier.
Better yet, you should strongly consider a liability umbrella insurance policy. A personal umbrella insurance policy covers negligence liability above the limits of your homeowner and car liability insurance policies. The minimum umbrella insurance coverage is typically $1,000,000. For example, if you cause $1,000,000 in medical damages to a person in an auto accident, but you only maintain auto insurance of $300,000, then your umbrella insurance policy will cover the additional $700,000 of liability.
Also, consider adding uninsured motorist coverage to your umbrella policy. If you have uninsured motorist coverage, your carrier will pay you the amount of damages you suffer from the negligence of an at-fault driver who has no or insufficient insurance. It costs significantly more to add uninsured motorist coverage to an umbrella policy. As a result, carriers typically do not include this coverage by default so that they can quote you a less expensive policy.
Malpractice Insurance
Asset protection should not substitute for a professional person’s adequate malpractice insurance. Sometimes professionals think that proper asset protection enables them to drop malpractice insurance. This is usually a mistake.
Asset protection does not make a person judgment proof. Most professionals do not want to live with a large judgment and have to rely on the long-term effectiveness of their asset protection plan. Asset protection laws change—an asset protection plan may become less effective during the life of a judgment because of future court rulings or legislative changes. Adequate insurance can solve a problem that could otherwise hamper the professional’s ability to practice efficiently and without an overhanging judgment.
The opposite is also true—malpractice insurance alone, without asset protection, is not sufficient for most professionals. Plaintiffs do not always settle for insurance limits, particularly when there are multiple defendants. In addition, sometimes a plaintiff’s attorney has promised their client a certain outcome, and the professional’s insurance limit is too low to meet that outcome. Finally, sometimes insurance carriers will refuse to cover liability, particularly if it is due to intentional actions, bad faith, or malicious conduct.
Most professionals should choose the highest malpractice insurance limit that they can afford. Also consider the following:
- Maintaining high limits allows a professional to insure events in the past, rather than having to get tail coverage.
- Some potential employees may decline to work for a firm that carries low or no insurance coverage.
- Ongoing litigation often results in an incredible amount of stress for the professional and their family, whether or not ultimately liable, and whether or not the professional has engaged in asset protection planning.
Liabilities Not Covered by Insurance
Some types of liabilities are not covered by insurance, even an umbrella policy. Asset protection is the only shield against non-insurable risks. These non-insurable risks include:
- Civil rights violations.
- Certain professional wrongdoing, such as bad faith or malicious conduct.
- Certain environmental liabilities.
- Criminal acts.
- Tax or other governmental liabilities.
Does Asset Protection Work?
Asset protection works best when implemented before any legal problems are on the horizon. Reorganization of asset titles and asset transfers done before creditor problems arise are effective.
Think of asset protection as legal insurance. Just like commercial insurance, asset protection works best when put in place before problems arise.
Unfortunately, just as most people do not visit a doctor until they experience illness or pain, most people do not consider asset protection until they feel vulnerable to creditor lawsuits.
Even after a potential claim arises, or even after a lawsuit is filed, asset protection planning is difficult but not impossible. Effective asset protection is possible until a judgment creditor obtains an interest in your property by lien or execution. Even late-implemented asset protection tools put the debtor in a better negotiating position.
Frequently Asked Questions
What assets are protected from creditors in Florida?
Florida law protects homestead property, retirement accounts, wages of head of household, and certain jointly owned assets from most creditors. Each category has specific rules and exceptions.
Can a Florida LLC protect personal assets from a lawsuit?
A properly structured multi-member Florida LLC can protect personal assets from liabilities of the business. However, personal guarantees or poor structuring can undermine protection.
Does Florida protect bank accounts from creditors?
Bank accounts owned as tenants by the entirety between spouses are protected from creditors of only one spouse. Individual accounts are not protected unless exempt by another law, such as wages of a head of household.
Can I lose my homestead to a creditor in Florida?
Florida’s homestead exemption protects a primary residence from most judgment creditors, with limited exceptions for taxes, mortgages, and certain liens.
Is asset protection legal in Florida?
Yes, asset protection is legal when not done as a fraudulent transfer. There are often strategies available even after a lawsuit or judgment is filed that do not constitute a fraudulent transfer.
When is it too late to protect my assets from creditors?
Once a creditor claim arises or a lawsuit is pending, any transfers may be considered fraudulent. Asset protection is most effective when done proactively.
What is the best way to protect assets in Florida?
There is no single best method. Common tools include the homestead exemption, LLCs, tenancy by the entirety, retirement accounts, and irrevocable trusts. The right strategy depends on the type of asset and status of any claims.
Can you use an offshore trust to protect assets in Florida?
Yes, offshore trusts offer the strongest asset protection available, and they can be set up even after a lawsuit or judgment is filed.
How does Florida’s tenancy by the entirety work for asset protection?
Assets jointly owned by a married couple as tenants by the entirety are protected from creditors of only one spouse. This includes real estate, bank accounts, and LLC interests.
What is a fraudulent transfer under Florida law?
A fraudulent transfer occurs when a debtor moves assets to avoid a creditor. Florida law allows creditors to undo such transfers made with intent to hinder, delay, or defraud.
Sign up for the latest information.
Get regular updates from our blog, where we discuss asset protection techniques and answer common questions.